The state still hasn’t provided guidance on who will be included in the next phase of the vaccine distribution plan
VANCOUVER — Time and patience.
Those two words sum up the best advice of state and local public health officials working to determine how COVID-19 vaccines will be doled out.
While the state initially estimated they would receive up to 400,000 doses of both the Pfizer and Moderna vaccines by the end of the month, the Department of Health now says it anticipates the actual number will be closer to 300,000.
Currently, the state is in the process of distributing vaccinations to people who qualify for Phase 1a. That includes between 300,000 and 500,000 frontline healthcare workers, paramedics and long-term care facility employees.
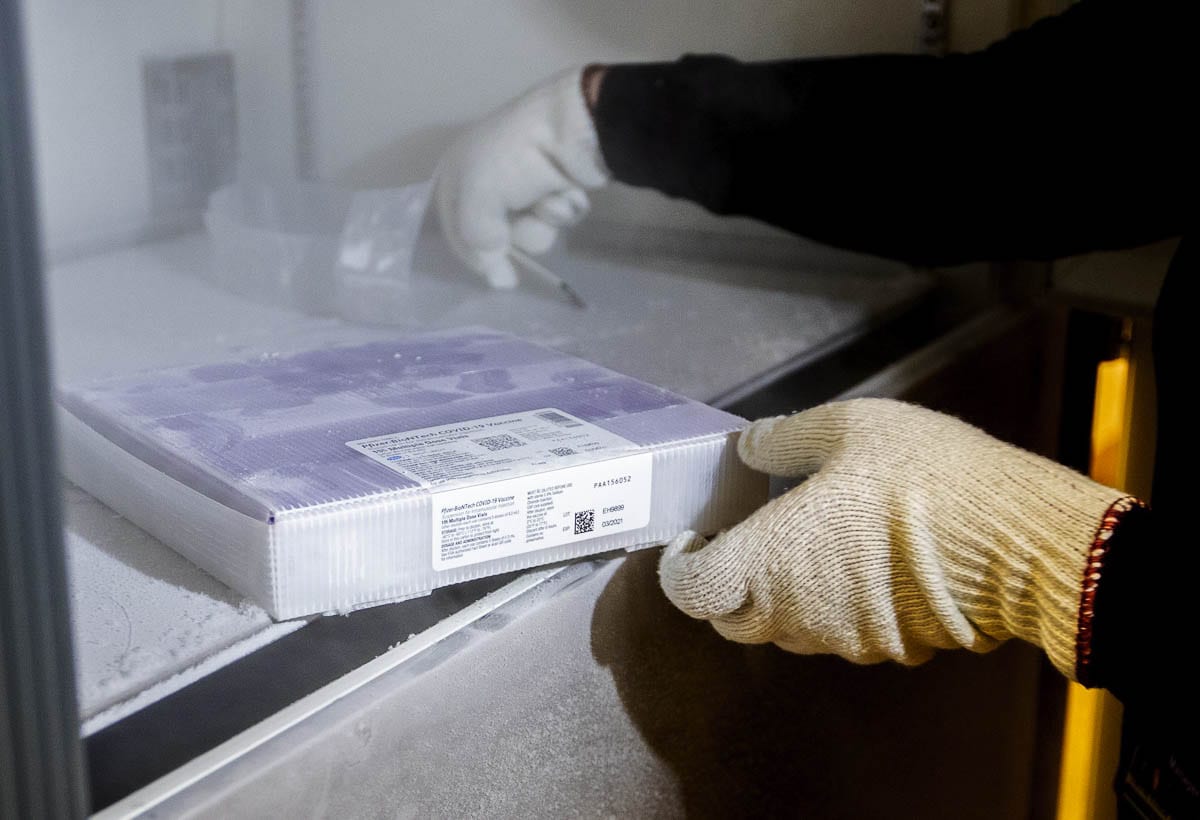
Since each vaccine requires two doses (21 days apart for the Pfizer vaccine and 28 days between Moderna doses), nearly a million total doses will be required just for the first phase.
With limited supplies of the vaccine available, hospitals around the state say they’ve had no shortage of medical workers willing to line up for a shot when they’re able to schedule it.
Prior to the arrival of the vaccines, several hospitals conducted polling of employees to see how many planned to receive the shots.
Somewhere around 55 percent said they planned to receive it as soon as possible, while a quarter intended to wait for more information. Almost 20 percent said they didn’t plan to get vaccinated at all, said Cassie Sauer, CEO of the Washington State Hospital Association (WSHA) last week.
But that equation may have shifted since the vaccines arrived.
“I think actually, ironically, the fact that it is such a scarce resource is increasing its appeal,” she added. “It’s sort of like the reservation you can’t get or the toy for your kids you can’t find. That seems to be making it more attractive.”
So far, no serious side effects from either vaccine have been reported in Washington state.
“I’ve had a little bit of a sore arm, but no other symptoms,” said Dr. Ellen Schur, director of clinical research at the University of Washington’s Diabetes Institute in Seattle. “I was able to go for a long walk the day I got it. And it was all, you know, pretty comforting.”
Others have reported some fatigue the day after receiving the vaccinations, but no allergic reactions or other serious side effects, although the second dose of each vaccine is said to carry a slightly higher risk of adverse reactions.
Even as the first shipments of vaccine are doled out around the state, and optimism increases that they might represent the beginning of the end of the pandemic, healthcare officials know plenty of work remains.
“One of my infection control nurses said getting the vaccine itself is like reaching base camp at Mount Everest,” said Schur. “Once you get that shot, you’re happy and excited. But it’s a long journey. It’s a lot of planning, it’s a lot of logistics.”
That will only become more pronounced once vaccine shipments pick up and the state issues guidance for who will be included in Phase 1b of the rollout.
“Scheduling is really challenging,” said Cassie Sauer, CEO of the Washington State Hospital Association (WSHA) during a media availability just before Christmas. “So the sooner we can know who’s in the 1b category, the sooner we can start reaching out to those people and getting them put on a schedule.”
The Centers for Disease Control recommends that Phase 1b include frontline essential workers, and people over the age of 75. The state can choose to follow those guidelines directly, or take its own path.
“It would be great to see law enforcement and teachers, grocery store workers and agricultural workers who are in these facilities that prepare and pack our food for us get some of the protection, as well,” said Dr. Francis Riedo, medical director of infectious disease at EvergreenHealth in Kirkland.
Once the vaccine is more broadly available, many pharmacies nationwide have already announced they will provide it free of charge through a partnership with the United States Department of Health and Human Services (HHS).
“I guess what I can say to the folks out there who feel like they’re in a very, very, very long line of millions of people waiting to get this vaccine, the front of the line is moving,” said Dr. Schur. “And it’s actually moving more quickly than we anticipated. So I find that really hopeful.”
In the meantime, health experts warn that it is far too soon to let up in our efforts to slow the spread of the virus.
While Washington is one of the few states with an agreement amongst all hospitals to share the load of patients in order to avoid crisis-level care, other parts of the country have struggled with overloaded emergency departments, full ICUs. In parts of Los Angeles County, patients were being wheeled on gurneys into gift shops due to a lack of space and some ambulances were turned away.
“We would have seen places like El Paso if we did not have that agreement,” said Sauer, who noted the eastern half of the state has been especially hard hit in recent weeks.
“Without significant intervention, we’re on pace to exceed the number of all the Americans that died in the Second World War probably in less than one year’s time,” warned Dr. Riedo, who was the first in the nation to document a case of community transmission during the first major outbreak at a Kirkland adult care home. “We’ve lost friends and co-workers, patients that we’ve cared for for years, and it’s something that can’t be denied.”
While many hospital systems have seen COVID-related hospitalizations back away from highs, the statewide total is still at the highest level since the beginning of the pandemic, showing that certain pockets of the state remain active hotbeds for the virus.
“The strain is less on actual beds than it is people to take care of the patients who are in the beds,” said Susan Stacey, chief nursing officer for Providence Sacred Heart Medical Center in Spokane. “We continue to have staffing challenges.”
While medical experts feel increasingly confident in their ability to limit fatalities from COVID-19, mortality rates have climbed in places where patient capacity is strained.
“Death from this disease is miserable. It is essentially suffocating alone, with very, very limited chance for family to be with you,” said Sauer. “So, for those who are dying, it’s a really challenging way to end their lives.”




